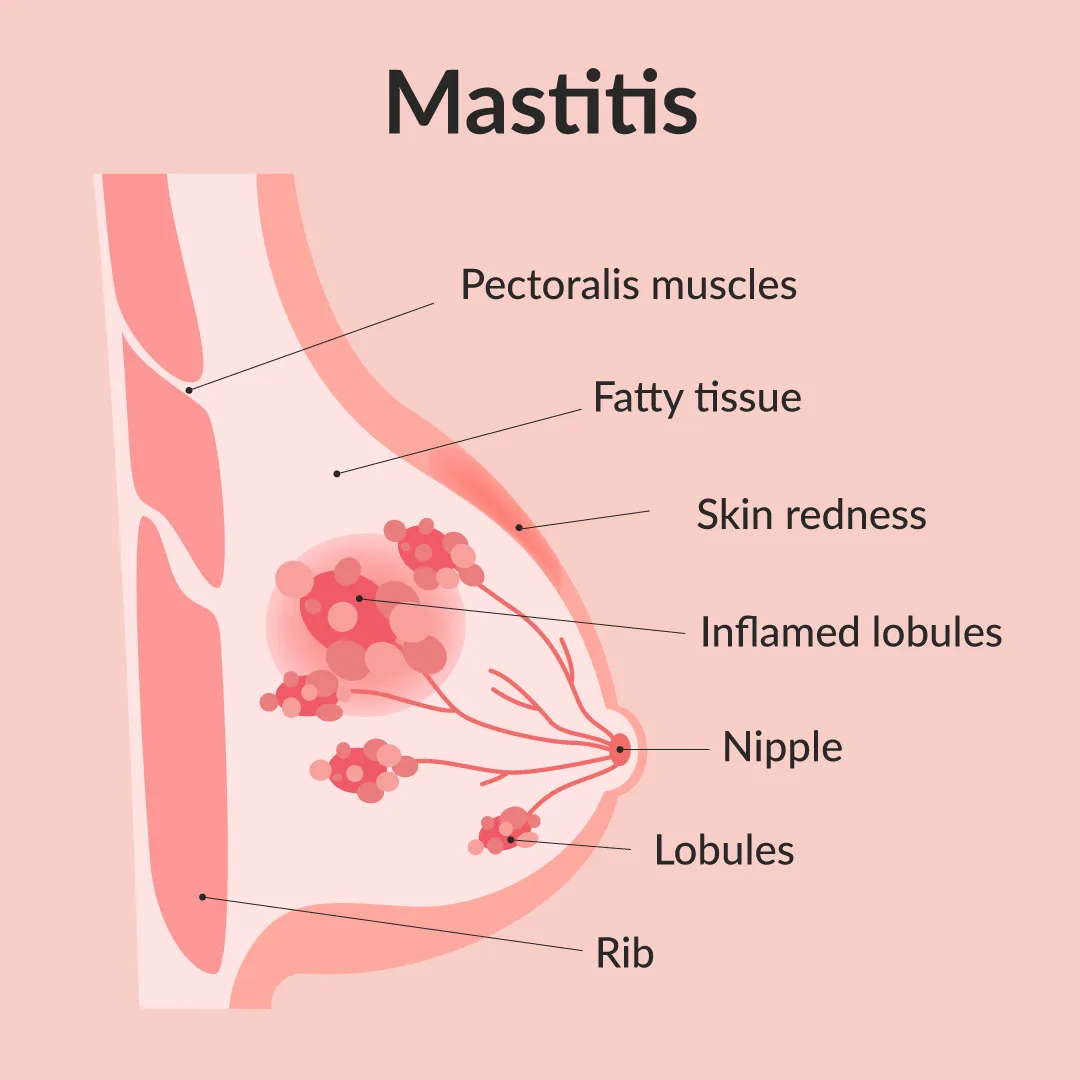
What is mastitis?
Mastitis is a condition characterized by inflammation in the breast, which can potentially result in an infection. It is most commonly observed in individuals who are breastfeeding. While mastitis can affect anyone, it is more frequently observed in women and individuals assigned female at birth (AFAB) who engage in breastfeeding (chestfeeding). However, it is important to note that men, individuals assigned male at birth (AMAB), and those who do not breastfeed can also develop mastitis, although such cases are relatively uncommon.
How common is mastitis?
Mastitis impacts approximately 10% of individuals who breastfeed in the United States and may affect as many as 30% of breastfeeding individuals globally. This condition is most frequently observed during the initial three months of breastfeeding.
What does mastitis look like?
Local symptoms may include:
- A tender, hot, painful area on the breast.
- Localized redness or red streaking.
- Localized firmness or swelling.
- Swollen axillary (armpit) lymph nodes on the respective side.
- Pain with breastfeeding or expressing.
- Clumpy or gelatinous milk.
- Pus or blood in milk.
Systemic symptoms may include:
- Fever (101°F or higher).
- Chills.
- Headache.
- General discomfort or feeling sick (malaise).
- Nausea.
- Muscle pain (myalgia).
- Decreased energy (lethargy), feeling fatigued.
Systemic symptoms may precede breast discomfort or may develop after your breast symptoms appear, and fever may be present even in cases of inflammatory mastitis.
What causes mastitis?
The primary cause of mastitis often stems from hyperlactation or an excessive milk supply. In such cases, the surplus milk can exert pressure on the milk ducts, causing them to narrow and resulting in engorgement, a condition where the breasts become significantly full and swollen. This specific condition is referred to as inflammatory mastitis.
Inflammatory mastitis, in turn, can escalate to bacterial mastitis, which occurs when infection develops as a consequence of inflammatory mastitis. On occasion, a bacterial infection can progress to form an abscess, which is a fluid collection that necessitates drainage.
What is the best treatment for mastitis?
The treatment for mastitis involves alleviating inflammation and pain while preventing the onset of infection. It is crucial to keep in mind that the field of lactation and mastitis is constantly evolving, so it’s essential to consult with your healthcare provider for the most current treatment guidance.
The primary cause of breast swelling is the inflammation of the structures surrounding the milk rather than a blockage of milk that needs to be expelled. Therefore, the focus should be on reducing inflammation to enhance milk flow.
At-home treatment for inflammatory mastitis includes:
- Ice: Apply an ice pack or a frozen bag of vegetables to reduce swelling while lying on your back to facilitate drainage into your lymph nodes. Heat application is discouraged.
- Pain relievers: Non-prescription nonsteroidal anti-inflammatory drugs (NSAIDS) like ibuprofen or naproxen can be used to diminish swelling and pain.
- Lymphatic drainage: Gently apply light pressure to your breast, similar to “petting a cat,” directing it towards the lymph nodes located above your collarbones and in your armpit. This technique aids in moving fluid and reducing swelling, but it should not be as forceful as a massage.
- Reverse pressure softening (RPS): RPS is a method to reduce swelling around your areola and nipple by redirecting fluid away from these areas. It facilitates easier latching for your baby. To perform RPS, position two fingertips at the base of your nipple, apply pressure, and then move your fingers away from the nipple, repeating this at different angles.
- Wear a supportive bra: Ensure that the bra you wear provides support without exerting excessive pressure on your breasts >> (Mamaway Maternity Bras).
What should NOT do:
- Avoid massaging your breasts.
- Do not use any type of massaging tools on your breast.
- Do not soak your breast in any substances.
- Avoid applying heat to the affected area.
How long does mastitis last?
Inflammatory mastitis typically resolves completely within a period of 10 to 14 days. When effectively managed, symptoms show significant improvement within 24 to 72 hours. Early recognition of engorgement and inflammation symptoms is crucial as it allows for the prompt initiation of treatment measures such as the use of ice and lymphatic drainage.
How can I prevent mastitis?
A good latch can potentially aid in preventing mastitis because your body can naturally regulate milk production in response to your baby’s milk consumption. If you are breastfeeding, there is no need to pump afterward in an attempt to “empty” your breast.
People who are breastfeeding can also take these steps to lower their chances of getting mastitis:
- Avoid wearing tight-fitting bras.
- Refrain from using nipple shells or similar devices on your breasts.
Source:


Leave a Reply